
以下内容原文发布于AACR官方博客《Cancer Research Catalyst》,中文内容仅做参考,请点击文末“阅读原文”,阅览原文内容。
本月编辑精选文章包含,一种预防多发性骨髓瘤患者接受免疫治疗感染的可能方法,Lynch综合征相关癌症的一组新的潜在生物标志物,模拟禁食饮食可以提高抗肿瘤免疫力的机制,等等。以下是所选研究的摘要。部分精选文章可限时免费在线阅览全文。
Journal: Blood Cancer Discovery
IVIg Use Associated with Ten-Fold Reduction of Serious Infections in Multiple Myeloma Patients Treated with Anti-BCMA Bispecific Antibodies
BCMA-targeted bispecific antibodies (BiAb) are efficacious in relapsed/refractory multiple myeloma; however, serious infections have emerged as important toxicities. In this retrospective study, we characterized all infections and their risk factors, and evaluated the impact of infection prophylaxis in patients treated with BCMA-targeted BiAbs. Among 37 patients, 15 (41%) experienced a grade 3–5 infection, with two infection-related deaths during deep remissions. Most (84%) infections occurred during disease remissions. The cumulative probability of grade 3–5 infection increased over time with no plateau. Among responders (n = 26), profound hypogammaglobulinemia occurred in 100% and continued throughout the entire duration of treatment. During periods when patients were receiving intravenous immunoglobulin (IVIg), the rate of grade 3–5 infections was 90% lower than during observation (incidence rate ratio, 0.10; 95% confidence interval, 0.01–0.80; P = 0.0307). No other risk factors for infection were identified. This study demonstrates that profound hypogammaglobulinemia is universal with BCMA-targeted BiAbs, with intravenous immunoglobulin potentially abrogating most of the infection risk.
Significance: To the best of our knowledge, this is the first study to comprehensively analyze risk factors and mitigation strategies to prevent infections in myeloma patients receiving anti-BCMA bispecific antibodies. Profound and prolonged hypogammaglobulinemia was universal among responders, while immunoglobulin replacement was associated with 90% lower rates of grade 3–5 infections.
Journal: Cancer Discovery
BCL2 Inhibition Reveals a Dendritic Cell–Specific Immune Checkpoint That Controls Tumor Immunosurveillance
We developed a phenotypic screening platform for the functional exploration of dendritic cells (DC). Here, we report a genome-wide CRISPR screen that revealed BCL2 as an endogenous inhibitor of DC function. Knockout of BCL2 enhanced DC antigen presentation and activation as well as the capacity of DCs to control tumors and to synergize with PD-1 blockade. The pharmacologic BCL2 inhibitors venetoclax and navitoclax phenocopied these effects and caused a cDC1-dependent regression of orthotopic lung cancers and fibrosarcomas. Thus, solid tumors failed to respond to BCL2 inhibition in mice constitutively devoid of cDC1, and this was reversed by the infusion of DCs. Moreover, cDC1 depletion reduced the therapeutic efficacy of BCL2 inhibitors alone or in combination with PD-1 blockade and treatment with venetoclax caused cDC1 activation, both in mice and in patients. In conclusion, genetic and pharmacologic BCL2 inhibition unveils a DC-specific immune checkpoint that restrains tumor immunosurveillance.
Significance: BCL2 inhibition improves the capacity of DCs to stimulate anticancer immunity and restrain cancer growth in an immunocompetent context but not in mice lacking cDC1 or mature T cells. This study indicates that BCL2 blockade can be used to sensitize solid cancers to PD-1/PD-L1–targeting immunotherapy.
Journal: Cancer Epidemiology, Biomarkers & Prevention
Long-term Cancer Survival Trends by Updated Summary Stage
Background: Stage is the most important prognostic factor for understanding cancer survival trends. Summary stage (SS) classifies cancer based on the extent of spread: In situ, Localized, Regional, or Distant. Continual updating of staging systems poses challenges to stage comparisons over time. We use a consistent summary stage classification and present survival trends for 25 cancer sites using the joinpoint survival (JPSurv) model.
Methods: We developed a modified summary stage variable, Long-Term Site-Specific Summary Stage, based on as consistent a definition as possible and applied it to a maximum number of diagnosis years, 1975–2019. We estimated trends by stage by applying JPSurv to relative survival data for 25 cancer sites in SEER-8, 1975–2018, followed through December 31, 2019. To help interpret survival trends, we report incidence and mortality trends using the joinpoint model.
Results: Five-year relative survival improved for nearly all sites and stages. Large improvements were observed for localized pancreatic cancer [4.25 percentage points annually, 2007–2012 (95% confidence interval, 3.40–5.10)], distant skin melanoma [2.15 percentage points annually, 2008–2018 (1.73–2.57)], and localized esophagus cancer [1.18 percentage points annually, 1975–2018 (1.11–1.26)].
Conclusions: This is the first analysis of survival trends by summary stage for multiple cancer sites. The largest survival increases were seen for cancers with a traditionally poor prognosis and no organized screening, which likely reflects clinical management advances.
Impact: Our study will be particularly useful for understanding the population-level impact of new treatments and identifying emerging trends in health disparities research.
Journal: Cancer Immunology Research
VISTA Expression on Cancer-Associated Endothelium Selectively Prevents T-cell Extravasation
Journal: Cancer Prevention Research
Methylated DNA Markers for Sporadic Colorectal and Endometrial Cancer Are Strongly Associated with Lynch Syndrome Cancers
Lynch syndrome (LS) markedly increases risks of colorectal and endometrial cancers. Early detection biomarkers for LS cancers could reduce the needs for invasive screening and surgical prophylaxis.
To validate a panel of methylated DNA markers (MDM) previously identified in sporadic colorectal cancer and endometrial cancer for discrimination of these cancers in LS.
In a case–control design, previously identified MDMs for the detection of colorectal cancer and endometrial cancer were assayed by qMSP on tissue-extracted DNA. Results were normalized to ACTB values within each sample. Least absolute shrinkage and selection operator models to classify colorectal cancer and endometrial cancer were trained on sporadic cases and controls and then applied to classify colorectal cancer and endometrial cancer, in those with LS, and cross-validated.
We identified colorectal cancer cases (23 with LS, 48 sporadic), colorectal controls (32 LS, 48 sporadic), endometrial cancer cases (30 LS, 48 sporadic), and endometrial controls (29 LS, 37 sporadic). A 3-MDM panel (LASS4, LRRC4, and PPP2R5C) classified LS-CRC from LS controls with an AUC of 0.92 (0.84–0.99); results were similar for sporadic colorectal cancer. A 6-MDM panel (SFMBT2, MPZ, CYTH2, DIDO1, chr10.4479, and EMX2OS) discriminated LS-EC from LS controls with an AUC of 0.92 (0.83–1.0); the AUC for sporadic endometrial cancer versus sporadic controls was nominally higher, 0.99 (0.96–1.0).
MDMs previously identified in sporadic endometrial cancer and colorectal cancer discriminate between endometrial cancer and benign endometrium and colorectal cancer and benign colorectum in LS. This supports the inclusion of patients with LS within future prospective clinical trials evaluating endometrial cancer and colorectal cancer MDMs and may provide a new avenue for cancer screening or surveillance in this high-risk population.
Journal: Cancer Research (May 1 issue)
Fasting-Mimicking Diet Drives Antitumor Immunity against Colorectal Cancer by Reducing IgA-Producing Cells
As a safe, feasible, and inexpensive dietary intervention, fasting-mimicking diet (FMD) exhibits excellent antitumor efficacy by regulating metabolism and boosting antitumor immunity. A better understanding of the specific mechanisms underlying the immunoregulatory functions of FMD could help improve and expand the clinical application of FMD-mediated immunotherapeutic strategies. In this study, we aimed to elucidate the role of metabolic reprogramming induced by FMD in activation of antitumor immunity against colorectal cancer. Single-cell RNA sequencing analysis of intratumoral immune cells revealed that tumor-infiltrating IgA+ B cells were significantly reduced by FMD treatment, leading to the activation of antitumor immunity and tumor regression in murine colorectal cancer models. Mechanistically, FMD delayed tumor growth by repressing B-cell class switching to IgA. Therefore, FMD-induced reduction of IgA+ B cells overcame the suppression of CD8+ T cells. The immunoregulatory and antitumor effects of FMD intervention were reversed by IgA+ B-cell transfer. Moreover, FMD boosted fatty acid oxidation (FAO) to trigger RUNX3 acetylation, thus inactivating Cα gene transcription and IgA class switching. IgA+ B-cell expansion was also impeded in patients placed on FMD, while B-cell expression of carnitine palmitoyl transferase 1A (CPT1A), the rate-limiting enzyme of FAO, was increased. Furthermore, CPT1A expression was negatively correlated with both IgA+ B cells and IgA secretion within colorectal cancer. Together, these results highlight that FMD holds great promise for treating colorectal cancer. Furthermore, the degree of IgA+ B cell infiltration and FAO-associated metabolic status are potential biomarkers for evaluating FMD efficacy.
Journal: Cancer Research (November 15 issue)
Stroma-Mediated Breast Cancer Cell Proliferation Indirectly Drives Chemoresistance by Accelerating Tumor Recovery between Chemotherapy Cycles
The ability of tumors to survive therapy reflects both cell-intrinsic and microenvironmental mechanisms. Across many cancers, including triple-negative breast cancer (TNBC), a high stroma/tumor ratio correlates with poor survival. In many contexts, this correlation can be explained by the direct reduction of therapy sensitivity induced by stroma-produced paracrine factors. We sought to explore whether this direct effect contributes to the link between stroma and poor responses to chemotherapies. In vitro studies with panels of TNBC cell line models and stromal isolates failed to detect a direct modulation of chemoresistance. At the same time, consistent with prior studies, fibroblast-produced secreted factors stimulated treatment-independent enhancement of tumor cell proliferation. Spatial analyses indicated that proximity to stroma is often associated with enhanced tumor cell proliferation in vivo. These observations suggested an indirect link between stroma and chemoresistance, where stroma-augmented proliferation potentiates the recovery of residual tumors between chemotherapy cycles. To evaluate this hypothesis, a spatial agent–based model of stroma impact on proliferation/death dynamics was developed that was quantitatively parameterized using inferences from histologic analyses and experimental studies. The model demonstrated that the observed enhancement of tumor cell proliferation within stroma-proximal niches could enable tumors to avoid elimination over multiple chemotherapy cycles. Therefore, this study supports the existence of an indirect mechanism of environment-mediated chemoresistance that might contribute to the negative correlation between stromal content and poor therapy outcomes.
Journal: Clinical Cancer Research (November 1 issue)
Regorafenib plus Vincristine and Irinotecan in Pediatric Patients with Recurrent/Refractory Solid Tumors: An Innovative Therapy for Children with Cancer Study
Purpose: This phase Ib study defined the safety, MTD, and recommended phase II dose (RP2D) of regorafenib combined with vincristine and irinotecan (VI). Secondary objectives were evaluation of antitumor activity and pharmacokinetics (PK) of regorafenib and irinotecan.
Patients and Methods: Patients aged 6 months to <18 years with relapsed/refractory solid malignancies [≥50% with rhabdomyosarcoma (RMS)] received regorafenib (starting dose 72 mg/m2/day) concomitantly or sequentially with vincristine 1.5 mg/m2 on days 1 and 8, and irinotecan 50 mg/m2 on days 1–5 (21-day cycle). Adverse events (AE) and tumor response were assessed. PK (regorafenib and irinotecan) were evaluated using a population PK model.
Results: We enrolled 21 patients [median age, 10 years; 12, RMS; 5, Ewing sarcoma (EWS)]. The MTD/RP2D of regorafenib in the sequential schedule was 82 mg/m2. The concomitant dosing schedule was discontinued because of dose-limiting toxicities in 2 of 2 patients treated. Most common grade 3/4 (>30% of patients) AEs were neutropenia, anemia, thrombocytopenia, and leukopenia. The overall response rate was 48% and disease control rate [complete response (CR)/partial response/stable disease/non-CR/non-progressive disease] was 86%. Median progression-free survival was 7.0 months [95% confidence interval (CI), 2.9–14.8] and median overall survival was 8.7 months (95% CI, 5.5–16.3). When combined with VI, regorafenib PK was similar to single-agent PK in children and adults (treated with regorafenib 160 mg/day).
Journal: Clinical Cancer Research (May 15 issue)
A Phase II Trial of Rivoceranib, an Oral Vascular Endothelial Growth Factor Receptor 2 Inhibitor, for Recurrent or Metastatic Adenoid Cystic Carcinoma
Purpose: This open-label, single-arm, phase II study evaluated the vascular endothelial growth factor receptor 2 (VEGFR2) tyrosine kinase inhibitor (TKI) rivoceranib in patients with recurrent or metastatic (R/M) adenoid cystic carcinoma (ACC).
Patients and Methods: Eligible patients had confirmed disease progression per Response Evaluation Criteria in Solid Tumors (RECIST) with ≥20% increase in radiologically or clinically measurable lesions or appearance of new lesions within the preceding 6 months. Patients received oral rivoceranib 700 mg once daily. Primary outcomes were objective response rate (ORR) by investigator review and by blinded independent review committee (BIRC).
Results: Eighty patients were enrolled and 72 were efficacy evaluable. Seventy-four patients had distant metastases and 49 received prior systemic treatment (14 received VEGFR TKIs). Per investigator and BIRC, respectively, ORR was 15.3% [95% confidence interval (95% CI), 7.9–25.7] and 9.7% (95% CI, 4.0–19.0); median duration of response was 14.9 months (95% CI, 4.9–17.3) and 7.2 months (95% CI, 3.5–8.4); and median progression-free survival was 9.0 months (95% CI, 7.3–11.5) and 9.0 months (95% CI, 7.7–11.5). Grade ≥3 treatment-related adverse events occurred in 56 patients (70.0%); the most common were hypertension (34, 42.5%) and stomatitis (6, 7.5%). Four grade 5 events occurred with one attributed to rivoceranib (epistaxis). Sixty-eight patients (85.0%) had ≥1 dose modifications and 16 patients (20.0%) discontinued rivoceranib for toxicity.
Journal: Molecular Cancer Research
USP1 Expression Driven by EWS::FLI1 Transcription Factor Stabilizes Survivin and Mitigates Replication Stress in Ewing Sarcoma
In this study, we identify USP1 as a transcriptional target of EWS::FLI1 and demonstrate the requisite function of USP1 in Ewing sarcoma (EWS) cell survival in response to endogenous replication stress. EWS::FLI1 oncogenic transcription factor drives most EWS, a pediatric bone cancer. EWS cells display elevated levels of R-loops and replication stress. The mechanism by which EWS cells override activation of apoptosis or cellular senescence in response to increased replication stress is not known. We show that USP1 is overexpressed in EWS and EWS::FLI1 regulates USP1 transcript levels. USP1 knockdown or inhibition arrests EWS cell growth and induces cell death by apoptosis. Mechanistically, USP1 regulates Survivin (BIRC5/API4) protein stability and the activation of caspase-9 and caspase-3/7 in response to endogenous replication stress. Notably, USP1 inhibition sensitizes cells to doxorubicin and etoposide treatment. Together, our study demonstrates that USP1 is regulated by EWS::FLI1, the USP1–Survivin axis promotes EWS cell survival, and USP1 inhibition sensitizes cells to standard of care chemotherapy.
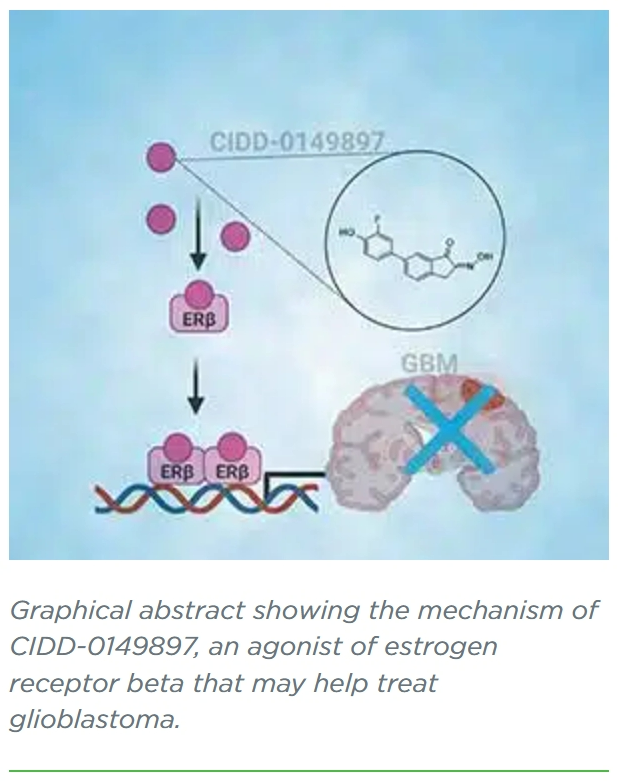
Journal: Molecular Cancer Therapeutics
Preclinical Development of Brain Permeable ERβ Agonist for the Treatment of Glioblastoma
Journal: Cancer Research Communications
Integrated Molecular Characterization of Intraductal Papillary Mucinous Neoplasms: An NCI Cancer Moonshot Precancer Atlas Pilot Project
Intraductal papillary mucinous neoplasms (IPMN) are cystic precursor lesions to pancreatic ductal adenocarcinoma (PDAC). IPMNs undergo multistep progression from low-grade (LG) to high-grade (HG) dysplasia, culminating in invasive neoplasia. While patterns of IPMN progression have been analyzed using multiregion sequencing for somatic mutations, there is no integrated assessment of molecular events, including copy-number alterations (CNA) and transcriptional changes that accompany IPMN progression. We performed laser capture microdissection on surgically resected IPMNs of varying grades of histologic dysplasia obtained from 23 patients, followed by whole-exome and whole-transcriptome sequencing. Overall, HG IPMNs displayed a significantly greater aneuploidy score than LG lesions, with chromosome 1q amplification being associated with HG progression and with cases that harbored co-occurring PDAC. Furthermore, the combined assessment of single-nucleotide variants (SNV) and CNAs identified both linear and branched evolutionary trajectories, underscoring the heterogeneity in the progression of LG lesions to HG and PDAC. At the transcriptome level, upregulation of MYC-regulated targets and downregulation of transcripts associated with the MHC class I antigen presentation machinery as well as pathways related to glycosylation were a common feature of progression to HG. In addition, the established PDAC transcriptional subtypes (basal-like and classical) were readily apparent within IPMNs. Taken together, this work emphasizes the role of 1q copy-number amplification as a putative biomarker of high-risk IPMNs, underscores the importance of immune evasion even in noninvasive precursor lesions, and reinforces that evolutionary pathways in IPMNs are heterogenous, comprised of both SNV and CNA-driven events.
Significance: Integrated molecular analysis of genomic and transcriptomic alterations in the multistep progression of IPMNs, which are bona fide precursors of pancreatic cancer, identifies features associated with progression of low-risk lesions to high-risk lesions and cancer, which might enable patient stratification and cancer interception strategies.
更多内容,请点击“阅读原文”
排版编辑:肿瘤资讯-Astrid











 苏公网安备32059002004080号
苏公网安备32059002004080号


