随着基因靶向治疗的适应证不断扩大,越来越多的乳腺癌患者通过主流肿瘤专科获得可遗传基因检测。不过,目前被检测的基因组合范围广泛,从BRCA1和BRCA2这两个最常见的乳腺癌易感基因,到包括多种癌症上百个基因的组合,随着基因检测数量越来越多,基因 检测费用也越来越贵。虽然有钱人不需要做选择题,可以全都要,但是如果检测到可遗传致病变异,最先被发现乳腺癌者以及其他家族性可遗传致病变异携带者可能都要接受干预措施,例如降低风险的双侧乳房切除手术甚至双侧卵巢和输卵管切除术以及针对该基因相关各种癌症进行数十年密切监测。那么,究竟哪些基因最值得先检测,目前仍然存在较大争议。
2025年6月15日,欧洲肿瘤内科学会官方期刊《肿瘤学年鉴》在线发表英国伦敦癌症研究院、曼彻斯特大学、埃克塞特大学、皇家德文郡和埃克塞特医院、剑桥大学、巴西西里奥利比亚医院、西班牙巴塞罗那大学希伯伦谷医院、马德里大学国庆日医院、意大利米兰大学欧洲肿瘤研究院、波兰波美拉尼亚医科大学、美国宾夕法尼亚大学、纽约纪念医院斯隆凯特林癌症中心、康奈尔大学威尔医学院、荷兰拉德堡德大学医学中心、澳大利亚皇家墨尔本医院彼得麦卡伦癌症中心、南非威特沃特斯兰德大学、新加坡国家癌症中心、南洋理工大学、德国慕尼黑大学、德国癌症联盟、加拿大麦吉尔大学联合起草的欧洲肿瘤内科学会精准肿瘤学工作组推荐意见,根据临床和公共卫生实际意义,对主流肿瘤专科乳腺癌可遗传多基因组合检测提出建议。
欧洲肿瘤内科学会精准肿瘤学工作组首先成立乳腺癌可遗传基因国际专家工作组,制定标准,用于评价每个乳腺癌易感基因是否可能被纳入乳腺癌多基因组合检测,从而为乳腺癌病例提供普遍适用的主流检测。随后,专家工作组对乳腺癌易感基因3个方面的影响进行评分:乳腺癌风险估计、临床可操作性、癌症相关死亡率。
结果,专家工作组一致同意,通过对癌症相关死亡率影响的可能性进行量化,确定乳腺癌多基因组合检测的临床和公共卫生实际意义。
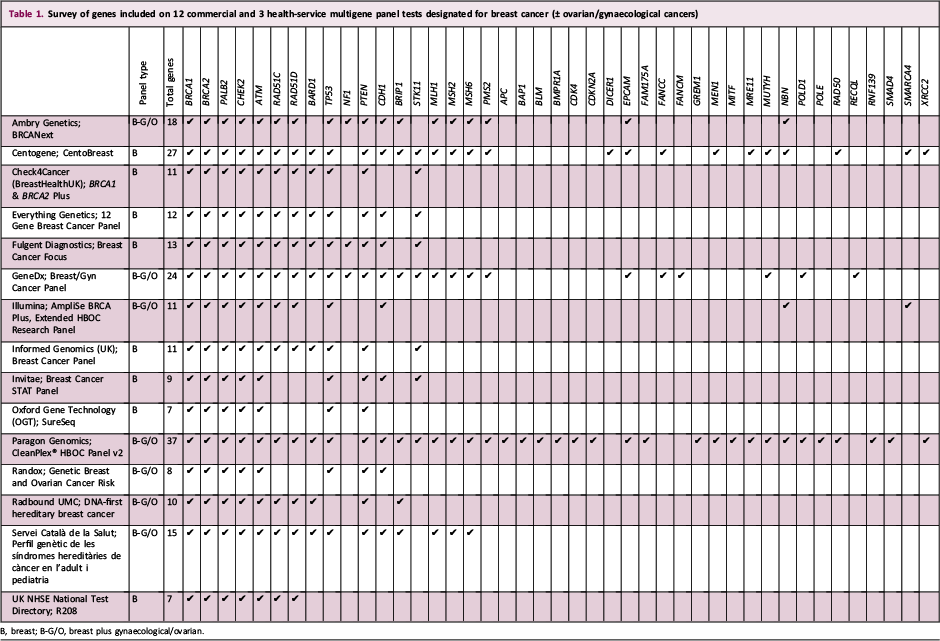

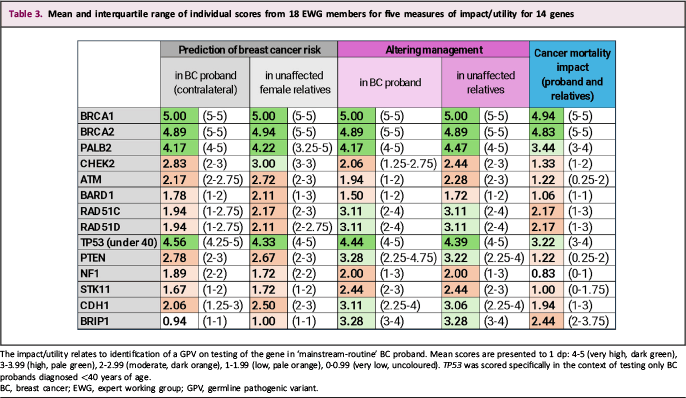
据此判断,6个乳腺癌易感基因被评定为具有中高度影响:BRCA1、BRCA2、PALB2、RAD51C、RAD51D、TP53(适用于乳腺癌被诊断时年龄小于40岁),并且可能加入BRIP1。
CHEK2和ATM具有中度影响,虽然可能有助于估计乳腺癌风险,但是被判定为不足以提供改善癌症相关死亡率的证据,并且主要用于雌激素受体阳性乳腺癌。
专家工作组强烈建议不要纳入“综合征”基因,例如STK11、PTEN、NF1、CDH1。这些基因不应急于检测,并且仅用于极少数乳腺癌病例。
因此,随着乳腺癌患者可遗传基因检测范围的扩大,以及在家族中进行的连锁检测,最终确定的可遗传致病变异携带者的数量和性质,将取决于最先被发现乳腺癌者多基因组合检测包括的基因。降低风险手术以及数十年对可遗传致病变异携带者进行多器官监测的潜在利弊和经济成本,应该通过癌症相关死亡率或者健康相关生活质量显著改善的强有力证据证明其合理性。

Ann Oncol. 2025 Jun 15. IF: 56.7
Breast cancer germline multigene panel testing in mainstream oncology based on clinical-public health utility: ESMO Precision Oncology Working Group recommendations.
Turnbull C, Achatz MI, Balmana J, Castro E, Curigliano G, Cybulski C, Domchek SM, Evans DG, Hanson H, Hoogerbrugge N, James PA, Krause A, Nathanson KL, Ngeow Yuen Yie J, Robson M, Tischkowitz M, Westphalen B, Foulkes WD.
The Institute of Cancer Research, London, UK; The University of Manchester, Manchester, UK; University of Exeter Medical School, Exeter, UK; Royal Devon University Healthcare NHS Foundation Trust, Exeter, UK; University of Cambridge, Cambridge, UK; Hospital Sírio-Libanês, Sao Paulo, Brazil; Vall d'Hebron Institute of Oncology (VHIO), Barcelona, Spain; Hospital Universitario Vall d'Hebron, Vall d'Hebron Hospital Campus, Barcelona, Spain; Hospital Universitario 12 de Octubre, Instituto de Investigación Sanitaria Hospital 12 de Octubre, Madrid, Spain; European Institute of Oncology, IRCCS, Milan, Italy; University of Milan, Milan, Italy; Pomeranian Medical University in Szczecin, Szczecin, Poland; University of Pennsylvania, Philadelphia, USA; Memorial Sloan Kettering Cancer Center, New York, USA; Weill Cornell Medical College, New York, USA; Radboud University Medical Center, Nijmegen, The Netherlands; The Royal Melbourne Hospital and Peter MacCallum Cancer Centre, Melbourne, Australia; The University of the Witwatersrand, Johannesburg, South Africa; National Cancer Centre Singapore, Singapore, Singapore; Nanyang Technological University, Singapore, Singapore; Ludwig-Maximilian University of Munich, Munich, Germany; German Cancer Consortium (DKTK Partner Site Munich), Heidelberg, Germany; McGill University, Montréal, Canada.
HIGHLIGHTS
ESMO Expert Working Group agreed a list of genes for inclusion on a BC-MGPT based on likely cancer-related mortality benefit
This BC-MGPT should include 7 genes: BRCA1, BRCA2, PALB2, RAD51C, RAD51D, BRIP1 and TP53 (for BC diag. <40 years).
This BC-MGPT is intended to service immediate diagnostic mainstreaming germline testing for all eligible BC cases.
'Syndromic' genes (e.g. STK11, PTEN, NF1, CDH1) should be tested later and only in a tiny minority of BC cases.
Mortality benefit was deemed equivocal for ATM and CHEK2, being of intermediate penetrance and primarily for ER-positive BC.
BACKGROUND : With widening therapeutic indications, germline genetic testing is offered to an increasing proportion of patients with breast cancer (BC) via mainstream oncology services. However, the gene set tested varies widely from just BRCA1/BRCA2 through to 'pan-cancer' panels of nearly 100 genes. If a germline pathogenic variant (GPV) is detected, the BC proband and other family GPV-carriers may be offered interventions such as risk-reducing surgery and intensive surveillance over decades for the various cancers linked to that gene.
METHODS : The European Society for Medical Oncology (ESMO) Precision Oncology Working Group established an international expert working group (EWG) in BC germline genetics. This EWG firstly established a framework of criteria by which to evaluate each breast cancer susceptibility gene (BCSG) for potential inclusion on a breast cancer multigene panel test (BC-MGPT) for universal mainstream testing for BC cases. Next, the EWG scored BCSGs for impact regarding (i) BC risk estimation, (ii) clinical actionability and (iii) cancer-related mortality.
RESULTS : The group agreed that they would constitute a BC-MGPT based on net clinical-public health utility, as quantified by likelihood of impact on cancer-related mortality. Judged as of high or moderate impact on this basis were six BCSGs: BRCA1, BRCA2, PALB2, RAD51C, RAD51D and TP53 (for BC diagnosed <40 years of age), with possible addition of BRIP1. While potentially informative for BC risk estimation, CHEK2 and ATM were judged to offer insufficient evidence for improving cancer-related mortality. The EWG recommended strongly against inclusion of 'syndromic' genes such as STK11, PTEN, NF1 and CDH1.
CONCLUSIONS : With expanded germline testing in patients with BC (and cascade testing into families), the number and nature of resultant GPV-carriers identified will be dictated by the genes included on the upfront BC-MGPT. The potential harms, opportunity and economic costs of decades of surveillance of multiple organs and risk-reducing surgeries for GPV-carriers should be justified by strong evidence of meaningful improvement in cancer-related mortality (or health-related quality of life).
KEY WORDS : breast cancer, multigene panel test, mainstream, germline, cancer-related mortality
DOI : 10.1016/j.annonc.2025.04.012











 苏公网安备32059002004080号
苏公网安备32059002004080号


