对于单侧乳腺癌女性,为了预防对侧乳腺癌,最彻底的办法是双侧乳房切除术。不过,双侧乳房切除术对于单侧乳腺癌女性死亡率的影响尚不明确。既往研究样本量较小,而且结果互相矛盾。
2024年7月25日,《美国医学会杂志》肿瘤学分册在线发表加拿大多伦多大学和女子学院医院的研究报告,根据初次手术类型对0至III期单侧乳腺癌女性20年乳腺癌死亡累积风险进行比较。
由于加拿大总人口不到4000万,于是加拿大人决定对隔壁总人口超过3亿的美国进行大数据分析。美国国家癌症研究所(NCI)监测、流行病学和最终结果(SEER)数据库从1973年开始收集全国癌症病例登记随访数据并且公开发布于其官方网站,目前已经覆盖全国超过三分之一人口。加拿大人首先从该数据库进行检索,2000年至2019年确诊单侧原发乳腺浸润癌或导管原位癌时年龄为30至79岁并且随访数据完整女性共计66万1270例,平均年龄58.7±11.3岁。再根据手术类型将这些女性分为3个治疗组:
乳房肿瘤切除术组:46万6756例 单侧乳房切除术组:15万4778例 双侧乳房切除术组:3万9736例
由于3个治疗组人数和特征分布悬殊,乳房肿瘤切除术人数最多、特征最好,双侧乳房切除术人数最少、特征最差,无法直接比较,故对不同特征进行2万次梯度提升机器迭代,得出倾向评分估计值最佳模型,随后根据诊断年份、诊断年龄、肿瘤大小分型分期分级、激素受体状态、HER2状态、种族、婚姻、家庭收入、居住地、放疗、化疗、随访年数、死亡原因等不同因素将这些女性按1比1比1进行倾向评分匹配,3个治疗组各计3万6028例女性,特征分布均衡。最后比较3组女性20年对侧乳腺癌发生率和乳腺癌死亡率。数据分析于2023年10月至2024年2月。
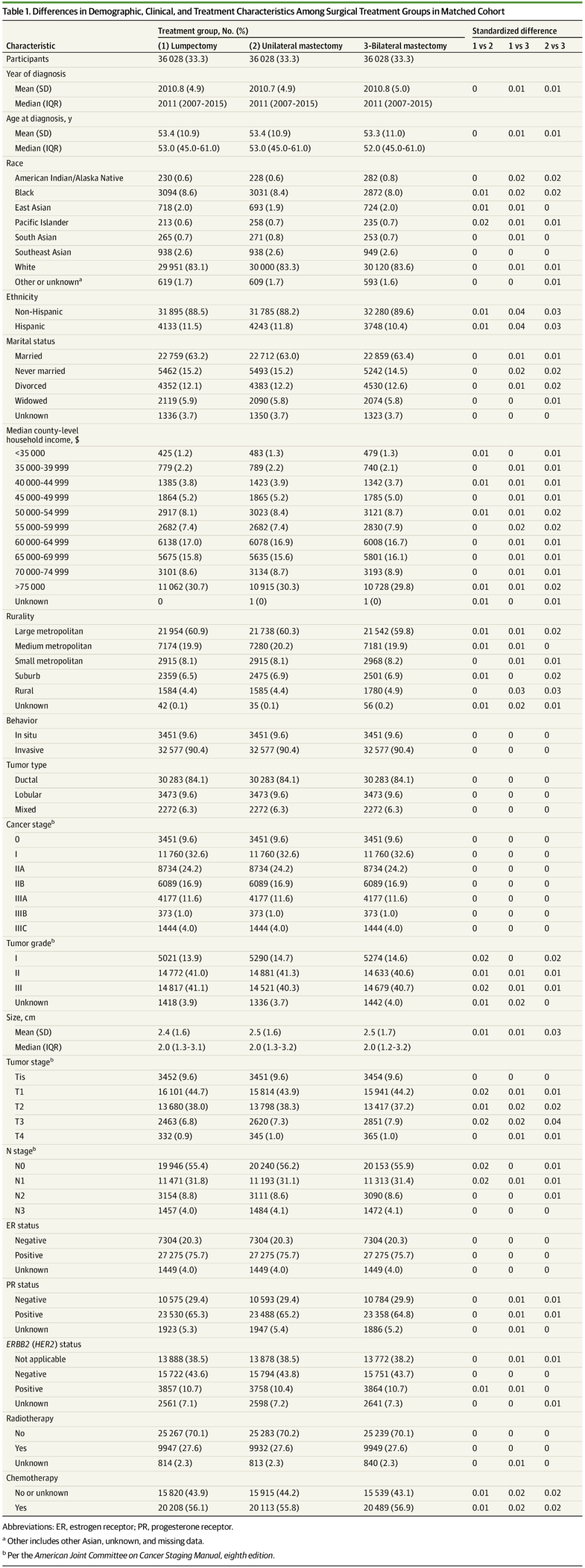
结果,20年随访期间,观察到1591例对侧乳腺癌:
乳房肿瘤切除术组:766例 单侧乳房切除术组:728例 双侧乳房切除术组:97例
乳房肿瘤切除术组与单侧乳房切除术组相比,20年对侧乳腺癌风险高6.9%(95%置信区间:6.1%~7.9%)。
发生与未发生对侧乳腺癌相比,15年乳腺癌累积死亡率为32.1%比14.5%(风险比:4.00,95%置信区间:3.52~4.54,以对侧乳腺癌为时间依赖性协变量)。
乳腺癌所致死亡人数:
乳房肿瘤切除术组:3077例(8.54%) 单侧乳房切除术组:3269例(9.07%) 双侧乳房切除术组:3062例(8.50%)
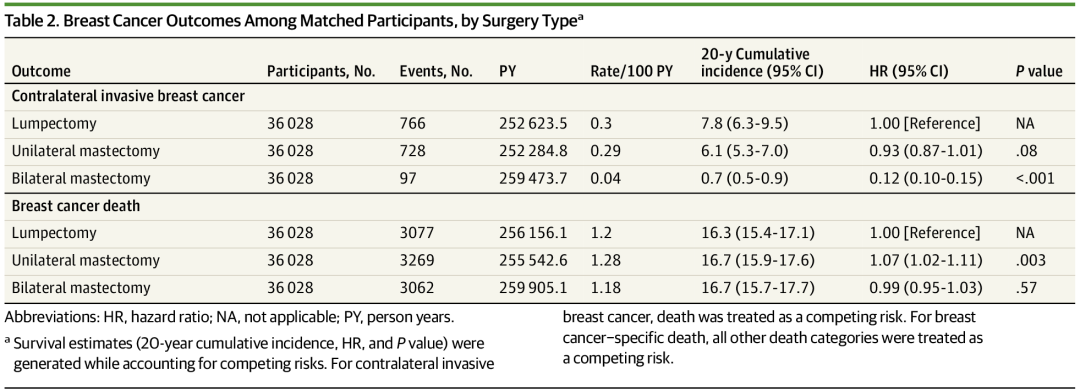
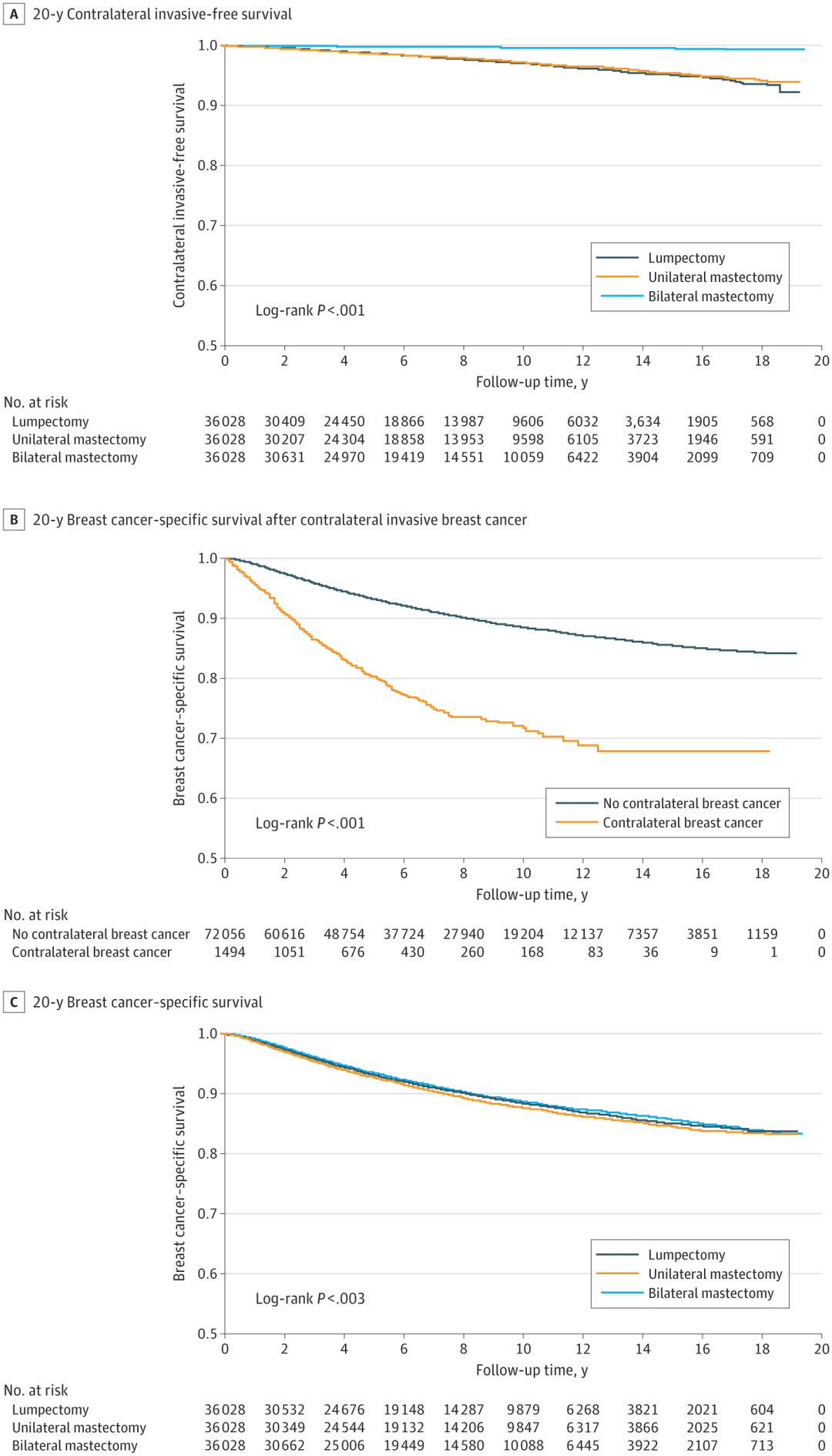
因此,该大样本队列长期随访研究结果表明,发生与未发生对侧乳腺癌相比,乳腺癌所致死亡风险大幅增加。双侧乳房切除术与乳房肿瘤切除术(保乳手术)和单侧乳房切除术相比,虽然对侧乳腺癌风险大大降低,但是乳腺癌所致死亡风险相似。对侧乳房切除术是预防对侧乳腺癌的有效手段,但是并未降低患者死于乳腺癌的风险,这使人们对新发对侧乳腺癌的转移潜力产生质疑。不过,该研究局限性在于SEER数据库缺少内分泌治疗、家族史、BRCA基因变异、乳腺癌筛查数据,无法对这些因素进行倾向评分匹配。
对此,芝加哥西北大学发表同期评论:对侧乳腺癌仍然是复杂的生物学难题。
JAMA Oncol. 2024 Jul 25. IF: 22.5
Bilateral Mastectomy and Breast Cancer Mortality.
Giannakeas V, Lim DW, Narod SA.
Women's College Hospital, Toronto, Ontario, Canada; University of Toronto, Toronto, Ontario, Canada.
QUESTION : Does bilateral mastectomy for treatment of unilateral breast cancer reduce the 20-year risk of breast cancer mortality?
FINDINGS : This cohort study including 661270 women with unilateral breast cancer who were closely matched by treatment type (lumpectomy, unilateral mastectomy, or bilateral mastectomy) and followed up for 20 years found that bilateral mastectomy was associated with a statistically significant reduction of contralateral breast cancer risk but not breast cancer mortality.
MEANING : These findings indicating that contralateral mastectomy for unilateral breast cancer is an effective means of cancer prevention but does not reduce the risk of dying of breast cancer call into question the metastatic potential of a de novo contralateral cancer.
IMPORTANCE : The benefit of bilateral mastectomy for women with unilateral breast cancer in terms of deaths from breast cancer has not been shown.
OBJECTIVES: To estimate the 20-year cumulative risk of breast cancer mortality among women with stage 0 to stage III unilateral breast cancer according to the type of initial surgery performed.
DESIGN, SETTINGS, AND PARTICIPANTS : This cohort study used the Surveillance, Epidemiology, and End Results (SEER) Program registry database to identify women with unilateral breast cancer (invasive and ductal carcinoma in situ) who were diagnosed from 2000 to 2019. Three closely matched cohorts of equal size were generated using 1:1:1 matching according to surgical approach. The cohorts were followed up for 20 years for contralateral breast cancer and for breast cancer mortality. The analysis compared the 20-year cumulative risk of breast cancer mortality for women treated with lumpectomy vs unilateral mastectomy vs bilateral mastectomy. Data were analyzed from October 2023 to February 2024.
EXPOSURES : Type of breast surgery performed (lumpectomy, unilateral mastectomy, or bilateral mastectomy).
MAIN OUTCOMES AND MEASURES : Contralateral breast cancer or breast cancer mortality during the 20-year follow-up period among the groups treated with lumpectomy vs unilateral mastectomy vs bilateral mastectomy.
RESULTS : The study sample included 661270 women with unilateral breast cancer (mean [SD] age, 58.7 [11.3] years). After matching, there were 36028 women in each of the 3 treatment groups. During the 20-year follow-up, there were 766 contralateral breast cancers observed in the lumpectomy group, 728 contralateral breast cancers in the unilateral mastectomy group, and 97 contralateral cancers in the bilateral mastectomy group. The 20-year risk of contralateral breast cancer was 6.9% (95% CI, 6.1%-7.9%) in the lumpectomy-unilateral mastectomy group. The cumulative breast cancer mortality was 32.1% at 15 years after developing a contralateral cancer and was 14.5% for those who did not develop a contralateral cancer (hazard ratio, 4.00; 95% CI, 3.52-4.54, using contralateral breast cancer as a time-dependent covariate). Deaths from breast cancer totaled 3077 women (8.54%) in the lumpectomy group, 3269 women (9.07%) in the unilateral mastectomy group, and 3062 women (8.50%) in the bilateral mastectomy group.
CONCLUSIONS AND RELEVANCE : This cohort study indicates that the risk of dying of breast cancer increases substantially after experiencing a contralateral breast cancer. Women with breast cancer treated with bilateral mastectomy had a greatly diminished risk of contralateral breast cancer; however, they experienced similar mortality rates as patients treated with lumpectomy or unilateral mastectomy.
PMID : 39052262
DOI : 10.1001/jamaoncol.2024.2212
JAMA Oncol. 2024 Jul 25. IF: 22.5
Contralateral Breast Cancer Remains a Complex Biologic Conundrum.
Khan SA, Kocherginsky M.
Northwestern University, Chicago, Illinois.
PMID : 39052310
DOI : 10.1001/jamaoncol.2024.2205











 苏公网安备32059002004080号
苏公网安备32059002004080号